New Study Links Controversial Gut Organism to Reduced Body Fat

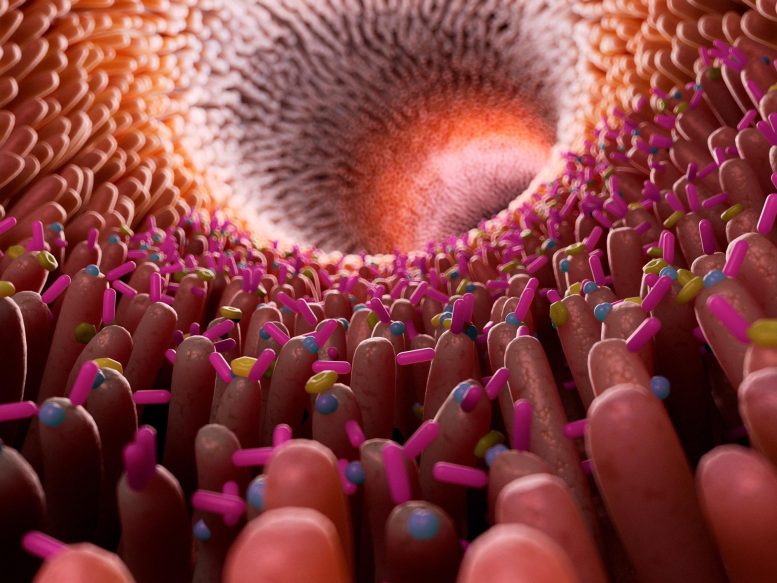
A global study involving over 50,000 participants links the presence of gut Blastocystis, traditionally seen as a parasite, with improved cardiovascular health and reduced body fat, suggesting beneficial effects on cardiometabolic health. Further research is required to validate these findings.
Research indicates elevated levels of Blastocystis in the intestines of individuals with improved cardiometabolic health and healthier dietary habits.
An international study, led by researchers from Massachusetts General Hospital (MGH), analyzed over 50,000 people globally and found that individuals carrying gut Blastocystis—a single-celled entity often considered either a parasite or a benign organism in the digestive system—were associated with signs of better cardiovascular health and reduced body fat. The findings were published in the journal Cell.
“Blastocystis’ effects on health and disease are controversial and likely context-dependent, but our research suggests that it may play a beneficial role in how diet impacts human health and disease,” said co-lead author Long H. Nguyen, MD, MS, a physician investigator in the Clinical and Translational Epidemiology Unit and Division of Gastroenterology at MGH, and an assistant professor of Medicine at Harvard Medical School. “At the very least, its ubiquity may suggest a non-pathogenic role.”
Nguyen, who is also a Chen Institute Department of Medicine Transformative Scholar at MGH, and colleagues sought to establish the relationship between gut Blastocystis, nutrition, and subsequent cardiometabolic health outcomes, including overweight/obesity, type 2 diabetes, and cardiovascular disease. To do so, they performed a large-scale study integrating and harmonizing data on nearly 57,000 individuals from 32 countries in North and South America, Europe, Asia, and Africa, focusing on Blastocystis and investigating whether its presence alters the effects of different dietary foods on individuals’ cardiometabolic health.
“We found that Blastocysis‘ presence and abundance varied by region and were influenced by diet,” said Nguyen.
Dietary Influence and Historical Presence
Blastocystis was associated with the intake of certain food items and overall dietary patterns favoring more healthful plant-based and minimally processed foods. Additionally, Blastocystis was hardly ever found in newborns, suggesting that it is likely acquired later in life and was even found in stool from 595 AD, suggesting it is not strictly a marker of a more modern microbiome configuration.
Notably, higher Blastocystis levels were linked to better short-term markers of cardiometabolic health. For example, the team observed more favorable blood sugar and lipid profiles in individuals with higher Blastocystis levels, suggesting a potential positive impact on cardiometabolic health beyond the effect of a healthy diet alone. Also, lower levels of Blastocystis were linked with long-term outcomes such as obesity.
Also, in adults who participated in a six-month personalized diet intervention study, improvements in diet quality were linked with subsequent increases in Blastocystis prevalence and abundance.
“Overall, our findings suggest a potentially beneficial modulating role for Blastocystis, which may help explain individualized responses to diet and differences in digestive health depending on the presence and level of Blastocystis,” said Nguyen. “Also, our results indicate that Blastocystis may not be a parasite with detrimental host effects but, rather, a favorable constituent of the human gut microbiome.”
Additional studies are needed to determine whether increasing Blastocystis levels represents a viable disease-prevention strategy, just as a growing number of studies are investigating the effects of modulating gut bacteria to fend off a range of medical conditions.
Reference: “Intestinal Blastocystis is linked to healthier diets and more favorable cardiometabolic outcomes in 56,989 individuals from 32 countries” by Elisa Piperni, Long H. Nguyen, Paolo Manghi, Hanseul Kim, Edoardo Pasolli, Sergio Andreu-Sánchez, Alberto Arrè, Kate M. Bermingham, Aitor Blanco-Míguez, Serena Manara, Mireia Valles-Colomer, Elco Bakker, Fabio Busonero, Richard Davies, Edoardo Fiorillo, Francesca Giordano, George Hadjigeorgiou, Emily R. Leeming, Monia Lobina, Marco Masala, Andrea Maschio, Lauren J. McIver, Mauro Pala, Maristella Pitzalis, Jonathan Wolf, Jingyuan Fu, Alexandra Zhernakova, Simone M. Cacciò, Francesco Cucca, Sarah E. Berry, Danilo Ercolini, Andrew T. Chan, Curtis Huttenhower, Tim D. Spector, Nicola Segata and Francesco Asnicar, 8 July 2024, Cell.
DOI: 10.1016/j.cell.2024.06.018
This work was supported by Zoe Ltd. and TwinsUK which is funded by the Wellcome Trust, Medical Research Council, Versus Arthritis, European Union Horizon 2020, Chronic Disease Research Foundation (CDRF), the National Institute for Health Research (NIHR) Clinical Research Network (CRN) and Biomedical Research Centre based at Guy’s and St Thomas’ NHS Foundation Trust in partnership with King’s College London. Additional funding information available in the publication.



